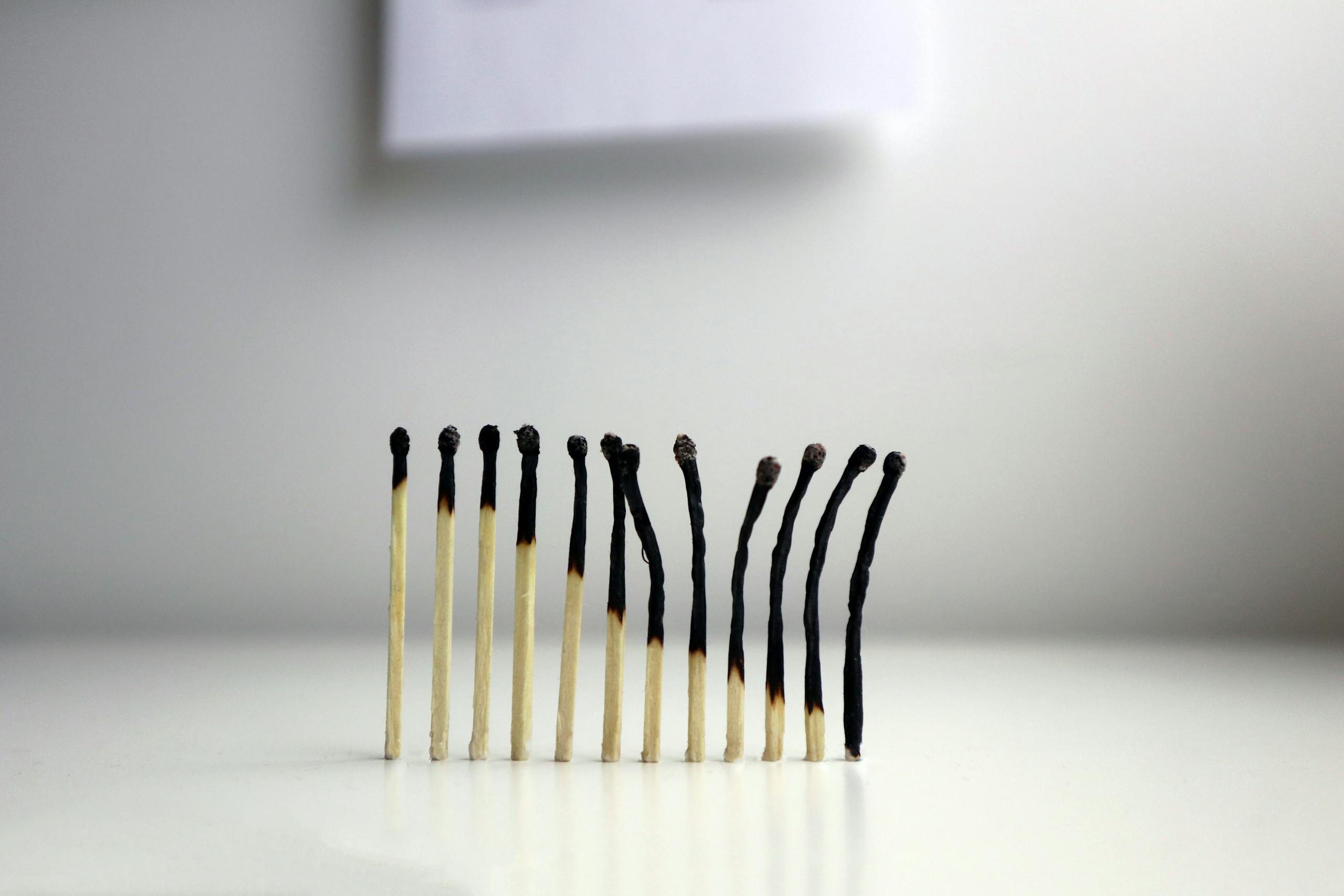
Forty-three percent of therapists report burnout within their first five years of practice. For ENTJs trained to help others, that statistic barely scratches the surface of a deeper tension. Building a career on strategic thinking, solving complex problems, and driving people toward measurable outcomes works brilliantly in most contexts. Then stepping into a therapy room reveals how everything that creates success can become the exact obstacle to therapeutic connection.

After two decades managing teams and consulting for Fortune 500 companies, I watched several ENTJ colleagues transition into counseling roles. Each one hit the same wall at roughly the same point. Their Te (Extraverted Thinking) wanted immediate, actionable solutions. Their clients needed space to process emotions without a five-step action plan. The cognitive functions that drove their professional success became obstacles to the very empathy their new role required.
ENTJs and ENTPs share similar patterns of strategic analysis and systems thinking. Our MBTI Extroverted Analysts hub addresses these personality patterns, and what emerges in therapeutic work reveals a specific challenge worth examining closely.
The Strategic Mind Meets Human Complexity
The ENTJ brain excels at pattern recognition. Walking into a therapy session often triggers immediate identification of three core issues, their interconnections, and a potential treatment trajectory. That’s not arrogance. According to the Myers & Briggs Foundation, Te-Ni (Extraverted Thinking supported by Introverted Intuition) creates a mental framework where efficiency and long-term vision intersect.
The problem surfaces when therapy doesn’t reward speed. Research from the American Psychological Association demonstrates that therapeutic outcomes correlate more strongly with the quality of the therapeutic alliance than with treatment modality or therapist credentials. Translation: the ability to sit with a client’s uncertainty matters more than solving their problems quickly.
During my consulting years, I worked with an ENTJ therapist who specialized in executive coaching. She could diagnose leadership gaps within a 30-minute intake session. Her clients valued her directness and strategic clarity. Then she pivoted to trauma work, and everything broke down. Trauma doesn’t follow a strategic roadmap. It loops, regresses, and resists linear progression. Her Te demanded structure. Her clients’ healing demanded patience.

The Efficiency Trap in Emotional Work
ENTJs optimize systems instinctively. You see inefficiencies and correct them. In business settings, that’s invaluable. In therapy, it creates a paradox. Emotions aren’t inefficient because they’re messy. They’re essential precisely because they resist optimization.
Consider how your cognitive functions process therapeutic interactions. Te wants to categorize symptoms, apply evidence-based interventions, and measure progress. Ni anticipates where the client’s issues will lead and prepares solutions before the client arrives at those insights themselves. Se (tertiary Extraverted Sensing) picks up on nonverbal cues but struggles to simply observe without interpreting. Fi (inferior Introverted Feeling) gets bypassed entirely because accessing personal emotional values feels like wading through fog compared to the clarity of logical analysis.
A 2018 study in the Journal of Counseling Psychology found that therapists with strong thinking preferences often show lower burnout rates in structured therapeutic modalities like CBT but higher burnout in person-centered or psychodynamic approaches. The data suggests cognitive style succeeds when the framework allows for strategic intervention but struggles when the work demands sustained emotional presence without clear endpoints.
Boundaries That Backfire
ENTJs establish boundaries effectively in most contexts. You protect your time, delegate appropriately, and maintain professional distance. In therapeutic settings, those same boundaries can create emotional walls that prevent genuine connection.
One colleague described her supervision sessions as exercises in cognitive dissonance. Her supervisor kept asking, “What did you feel when the client said that?” She kept answering with what she thought, what she assessed, what intervention she planned to deploy. The supervisor wasn’t looking for analysis. She wanted emotional attunement. My colleague’s boundaries weren’t the problem. Her automatic default to strategic thinking was.

The tension intensifies because ENTJs often enter helping professions from a place of competence. You’ve mastered other domains. You expect to master this one too. But therapy demands something different from mastery. It requires vulnerability, not as a weakness to overcome but as a tool for connection. Your Te resists that framework because vulnerability doesn’t optimize anything. It just exists.
The Competence-Compassion Divide
ENTJs demonstrate compassion through action. You help people by solving their problems, removing obstacles, and creating pathways to success. That form of compassion works in management, mentorship, and strategic advising. It fails in therapy because therapeutic compassion isn’t transactional. It doesn’t produce immediate, measurable results.
Stanford’s Center for Compassion and Altruism Research and Education examined how different personality types express empathy in clinical settings. Those with strategic thinking preferences scored high on “cognitive empathy” (understanding someone’s perspective intellectually) but lower on “affective empathy” (feeling what someone else feels). The research noted that cognitive empathy alone often led to well-intentioned but emotionally disconnected interventions.
Understanding a client’s pain intellectually comes naturally. Mapping its origins, identifying maintaining factors, and prescribing evidence-based treatments follows logically. What creates difficulty is sitting in that pain without rushing to fix it. Ni sees the endpoint. Te wants to build the bridge. The client needs acknowledgment that they’re standing in difficult terrain before solutions get constructed.
Success Metrics That Don’t Apply
How do you measure therapeutic success as an ENTJ? Your professional background taught you to track KPIs, conversion rates, and outcome metrics. Therapy offers symptom reduction scales, treatment plan progress notes, and session attendance rates. None of those capture what actually happens in the room.
A client might show up for six months, complete all homework assignments, and report minimal symptom improvement on standardized measures. Then in session 24, they mention a small shift in how they relate to their partner. That shift doesn’t show up in your outcome data. It doesn’t fit your strategic plan. But it represents meaningful change.
ENTJs in therapy often experience a specific form of professional doubt. You’re accustomed to clear feedback loops. You implement a strategy, measure results, adjust based on data. Therapy provides ambiguous feedback. A client says they feel better, but their behavior hasn’t changed. Another client reports increased distress but demonstrates more emotional awareness. Which outcome matters more? Your Te demands clarity that the work doesn’t provide.
The Hidden Cost of Clinical Detachment
Professional boundaries require some emotional distance. ENTJs excel at maintaining that distance. Client issues don’t follow them home. Compartmentalization works effectively. Professional identity stays separate from personal reactions.
Those protective mechanisms serve you well until they don’t. Studies in the Journal of Clinical Psychology found that therapists who maintained rigid emotional boundaries reported lower rates of acute stress but higher rates of existential burnout. They weren’t overwhelmed by individual cases. They were slowly depleting their capacity for genuine connection.
One ENTJ therapist I consulted with described feeling like she was “performing empathy” rather than experiencing it. She hit all the right clinical markers: reflective listening, appropriate self-disclosure, emotional validation. Her supervisors praised her technique. Her clients completed treatment. She felt increasingly hollow. The strategic execution of therapeutic presence isn’t the same as being present. Her Te could mimic connection. Her Fi knew the difference.
When Pattern Recognition Becomes Pattern Imposition
Your Ni-Te combination sees patterns everywhere. That’s valuable in diagnostic work, case conceptualization, and treatment planning. It becomes problematic when you start imposing patterns on clients who don’t fit your framework.
A client presents with relationship difficulties. You recognize the pattern: anxious attachment stemming from inconsistent early caregiving, leading to protest behavior in adult relationships. You design interventions targeting attachment security. The client doesn’t improve because their relationship issues stem from undiagnosed ADHD, not attachment trauma. Your pattern recognition was correct for a different case. It didn’t apply here.

ENTJs typically course-correct quickly when presented with contradicting data. In therapy, the data arrives slowly and ambiguously. A client might improve for reasons unrelated to your interventions. Another might deteriorate despite evidence-based treatment. Your strategic mind wants clear cause-effect relationships. The therapeutic process rarely provides them.
Redesigning Your Approach Without Abandoning Your Strengths
The solution isn’t suppressing your ENTJ characteristics. You can’t excise your cognitive functions. You can, however, deploy them differently.
Te creates structure. Apply it to clinical frameworks, not to clients’ emotional experiences. Design intake processes that gather comprehensive data. Build treatment protocols that allow for flexibility within structure. Strategic thinking can create space for ambiguity rather than eliminate it.
Ni anticipates outcomes. Let this function inform long-term treatment vision without dictating session-by-session expectations. Holding both a strategic treatment arc and immediate therapeutic presence works because they operate at different timescales.
Inferior Fi represents the greatest therapeutic asset and biggest challenge for ENTJs. It holds personal values, emotional authenticity, and capacity for deep connection. Access requires slowing down dominant functions enough to notice what you actually feel, not just what you think about feelings.
Several ENTJs I’ve worked with found success by treating their Fi development as a strategic priority. Regular supervision focused specifically on emotional awareness became part of their professional routine. Mindfulness practice served not as a therapeutic technique for clients but as a method for accessing their own emotional landscape. Fi activation got tracked the same way treatment outcomes were measured.
Matching Modality to Cognitive Strengths
Not all therapeutic approaches suit ENTJ cognitive functions equally. Modalities that emphasize structure, measurement, and strategic intervention align more naturally with your processing style.
Cognitive Behavioral Therapy provides clear protocols, measurable outcomes, and evidence-based interventions. Strategic thinking thrives in that framework. Solution-Focused Brief Therapy leverages goal orientation and systematic analysis. Acceptance and Commitment Therapy combines behavioral activation with values work, engaging both logical thinking and emotional awareness development.
Person-centered therapy demands sustained emotional presence without directive intervention. Psychodynamic work requires comfort with ambiguity and unconscious process. ENTJs can excel in these modalities, but they require deliberate Fi development and willingness to sit with uncertainty. That’s not impossible. It’s just not your default mode.
Consider what drew you to therapy in the first place. Attraction to the intellectual challenge of understanding human behavior might indicate research or assessment-focused work suits cognitive strengths better than ongoing clinical practice. Those who value seeing measurable client progress will find short-term, goal-oriented modalities more aligned with their preferences. Genuine interest in emotional depth work requires investment in Fi development as a core professional competency, not just a supplementary skill.
The Supervision Mismatch
Many therapy supervision models emphasize emotional processing and relational dynamics. ENTJ supervisees often report feeling misunderstood in supervision. Your supervisor asks about your feelings toward a client. You respond with your clinical assessment. Your supervisor interprets that as defensiveness or lack of insight. You experience it as answering a different question than the one they asked.
Effective supervision for ENTJs requires explicit translation between your cognitive style and your supervisor’s expectations. Ask directly: “Are you asking how I feel emotionally, or are you asking for my clinical impression?” Clarify whether emotional self-disclosure is optional or required for the supervision process. Request concrete examples of what “sitting with discomfort” looks like in practice rather than abstract directives to “be more present.”
One ENTJ therapist I consulted with switched supervisors three times before finding someone who understood how to work with her cognitive style. Her effective supervisor didn’t ask her to suppress her Te. Instead, he helped her use Te to develop Fi. They created structured exercises for emotional awareness. They tracked her Fi engagement like any other clinical skill. The supervision became a strategic process for developing emotional competence rather than an implicit criticism of her natural processing style.
Client Selection and Setting Boundaries
ENTJs often struggle with saying no to clients who need services outside their area of competence. Your competence-oriented mindset assumes you should be able to help everyone. That’s not how therapy works.
Clients experiencing acute emotional crises without clear behavioral goals might drain your resources more than clients with specific, actionable problems. That doesn’t make you a bad therapist. It means your cognitive strengths align better with certain clinical presentations. Recognizing that allows you to build a caseload that sustains you rather than depletes you.
Setting boundaries means declining referrals that don’t fit your therapeutic style, even when you have availability. It means referring clients to colleagues better suited to their needs, even when that feels like admitting limitation. Your Te might interpret referrals as failure. Your developing Fi recognizes that matching clients with appropriate therapists serves everyone better than forcing a mismatched therapeutic relationship.
Explore more perspectives on ENTJ communication patterns, when ENTJ strengths become liabilities, working under ENTJ leadership, what makes ENTJ leadership effective, and ENTJ professional burnout patterns.
Explore more ENTJ and ENTP insights in our complete MBTI Extroverted Analysts hub.
About the Author
Keith Lacy is an introvert who’s learned to embrace his true self later in life. After spending over 20 years in corporate marketing and creative agency leadership, Keith started Ordinary Introvert to share research-backed insights on introversion, MBTI personality types, relationships, mental health, and career development. His work combines real-world experience with practical strategies grounded in personality science.
Frequently Asked Questions
Can ENTJs be successful therapists?
Yes, ENTJs can excel as therapists, particularly in modalities that align with their strategic thinking and goal orientation. Success requires developing emotional awareness (Fi function) and choosing therapeutic approaches that complement rather than contradict their cognitive strengths. Many ENTJs thrive in CBT, solution-focused therapy, or specialized areas like executive coaching where structure and measurable outcomes play central roles.
Why do ENTJs struggle with emotional presence in therapy?
ENTJs default to Te (Extraverted Thinking) and Ni (Introverted Intuition), which prioritize logical analysis and strategic planning over emotional processing. Their inferior Fi (Introverted Feeling) makes accessing personal emotional values less automatic. In therapy, this creates tension between wanting to solve problems efficiently and needing to provide sustained emotional attunement without rushing to solutions.
What therapeutic modalities work best for ENTJ therapists?
Structured, evidence-based modalities like Cognitive Behavioral Therapy, Solution-Focused Brief Therapy, and Acceptance and Commitment Therapy align well with ENTJ cognitive functions. These approaches provide clear protocols, measurable outcomes, and strategic intervention opportunities. Less structured modalities like psychodynamic or person-centered therapy require more deliberate Fi development to avoid defaulting to premature problem-solving.
How can ENTJs develop their inferior Fi for therapeutic work?
Treat Fi development as a strategic competency requiring deliberate practice. Schedule regular supervision focused on emotional awareness, practice mindfulness to access your emotional landscape, and track Fi engagement like any measurable skill. Create structured exercises for identifying and expressing feelings, and work with supervisors who understand how to bridge Te-dominant processing with Fi development needs.
What causes burnout specifically for ENTJ therapists?
ENTJ therapists often experience burnout from the mismatch between their efficiency-oriented cognitive style and therapy’s inherently ambiguous, slow-moving process. Rigid emotional boundaries protect against acute stress but create existential depletion over time. The constant effort to suppress natural problem-solving instincts in favor of emotional presence drains energy without providing the clear success metrics ENTJs use to validate their competence.







