INFPs facing a prostate cancer diagnosis experience unique emotional and psychological challenges that differ from other personality types. Their deep need for authenticity, intense processing of emotions, and tendency toward introspection can both complicate and strengthen their healing journey in unexpected ways.
As someone who’s spent decades working with diverse personality types in high-pressure environments, I’ve seen how INFPs approach major life challenges differently. Their rich inner world becomes both sanctuary and battleground when confronting serious health issues like cancer.

Understanding how INFP cognitive functions interact with cancer treatment, emotional processing, and recovery decisions can make the difference between feeling overwhelmed and finding meaning in the experience. Our MBTI Introverted Diplomats hub explores the full spectrum of INFP experiences, but health challenges reveal aspects of this personality type that remain hidden during ordinary circumstances.
How Do INFPs Process a Cancer Diagnosis Differently?
The INFP’s dominant function, Introverted Feeling (Fi), creates an immediate and intense emotional response to a cancer diagnosis. Unlike other types who might focus on logistics or seek external reassurance, INFPs turn inward first. They need time to process what this means for their identity, values, and life purpose.
This internal processing can look like withdrawal to family members and medical teams. Where an ENFJ might immediately start building support networks and an ESTJ might dive into research and treatment plans, INFPs often need solitude to understand their authentic response to the diagnosis.
During my years managing client relationships, I learned that INFPs don’t make decisions the same way other types do. They can’t simply weigh pros and cons on a spreadsheet. Every treatment option must align with their core values and sense of personal authenticity. This isn’t stubbornness, it’s how their cognitive architecture works.
The auxiliary function, Extraverted Intuition (Ne), adds another layer of complexity. INFPs see multiple possibilities and potential meanings in their diagnosis. They might explore alternative treatments, research holistic approaches, or spend significant time considering how cancer fits into their life narrative. This can frustrate medical professionals who prefer straightforward treatment compliance.
What Emotional Challenges Do INFPs Face During Treatment?
INFPs experience cancer treatment as more than a medical process. It becomes an existential journey that challenges their fundamental beliefs about life, meaning, and personal identity. The structured, protocol-driven nature of oncology care can feel dehumanizing to someone whose dominant function prioritizes individual authenticity.

The loss of control inherent in cancer treatment particularly affects INFPs. Their need for autonomy and self-direction conflicts with the reality of scheduled treatments, side effects, and medical supervision. This can trigger their tertiary function, Introverted Sensing (Si), in unhealthy ways, causing them to ruminate on past health decisions or become hyperfocused on physical symptoms.
Emotional overwhelm is common during treatment phases. INFPs feel everything deeply, including the fear, sadness, and anger that accompany cancer. However, their tendency to internalize emotions can prevent them from seeking appropriate support. They might worry about burdening others or struggle to articulate their complex emotional landscape.
I’ve observed that INFPs often experience what I call “meaning-making fatigue” during treatment. Their Ne function constantly searches for significance and patterns, but cancer’s unpredictability can exhaust this natural tendency. They might oscillate between finding profound meaning in their experience and feeling completely lost.
The medical environment itself presents challenges. INFPs prefer authentic, personal connections but often encounter rushed appointments, clinical language, and impersonal treatment protocols. This disconnect can increase their sense of isolation during an already vulnerable time.
How Can INFPs Build Effective Support Systems?
Traditional support group models often don’t work well for INFPs. Large groups with structured sharing can feel artificial and draining. Instead, INFPs benefit from one-on-one connections with people who understand their need for authentic communication and emotional depth.
Quality matters more than quantity for INFP support networks. They need a few close friends or family members who can sit with their emotions without trying to fix or minimize them. These supporters should understand that INFPs process externally through conversation but need time between discussions to integrate insights internally.
Creative expression becomes crucial during treatment. INFPs might find more healing in art therapy, journaling, or music than in traditional talk therapy. These outlets allow them to process complex emotions and maintain connection to their authentic selves when medical treatment feels dehumanizing.
Professional counseling should align with INFP preferences. They respond better to therapists who use person-centered or existential approaches rather than cognitive-behavioral techniques. The therapeutic relationship itself matters as much as specific interventions.

Online communities can provide valuable support when chosen carefully. INFPs often connect better through written communication where they can craft thoughtful responses. Forums focused on meaning-making, spirituality, or creative expression during illness might resonate more than purely medical support groups.
What Decision-Making Strategies Work Best for INFPs?
INFPs need time and space to make treatment decisions that align with their values. Rushed medical decisions can create lasting internal conflict, even when the clinical outcome is positive. Healthcare providers should understand that INFPs aren’t being difficult when they need extended time to consider options.
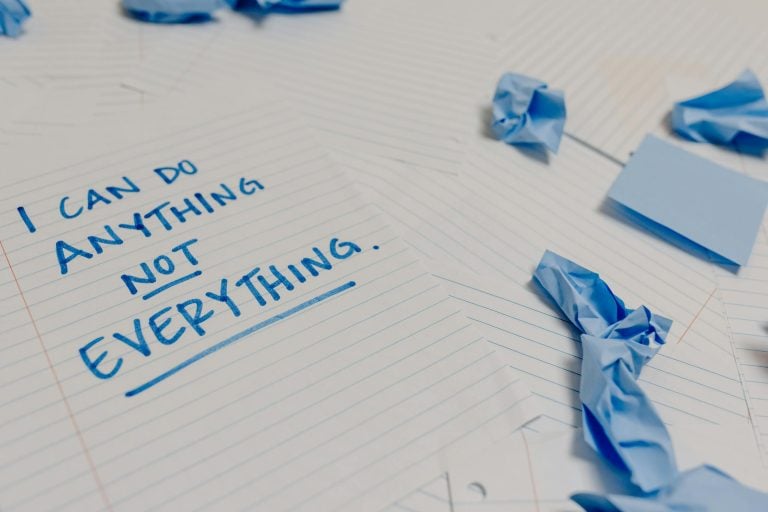
Values clarification becomes essential. INFPs should explicitly identify what matters most to them: quality of life, family time, maintaining independence, pursuing creative projects, or spiritual growth. These values become the filter through which all treatment decisions pass.
The Ne function helps INFPs see creative treatment combinations and alternative approaches. They might benefit from integrative oncology programs that combine conventional treatment with complementary therapies. This allows them to maintain some sense of personal agency while receiving necessary medical care.
Decision-making tools should accommodate INFP cognitive preferences. Instead of purely analytical pros-and-cons lists, they might create vision boards, write letters to their future self, or use guided imagery to explore how different choices feel emotionally and spiritually.
Involving trusted advisors in decision-making helps INFPs process externally while maintaining autonomy. They benefit from discussing options with people who understand their values and can help them identify when fear or pressure might be clouding their judgment.
How Do INFPs Find Meaning in Their Cancer Experience?
For INFPs, cancer isn’t just a medical condition to overcome. It becomes part of their life story, requiring integration into their sense of identity and purpose. This meaning-making process is crucial for their psychological well-being and can significantly impact their treatment adherence and recovery.
Many INFPs discover that cancer strips away superficial concerns and clarifies what truly matters. This aligns with their natural tendency toward authenticity. They might use their diagnosis as an opportunity to align their life more closely with their core values, even making significant changes in relationships, career, or lifestyle.

The experience often awakens or deepens spiritual exploration. INFPs might find themselves questioning previous beliefs, exploring new spiritual practices, or developing a more personal relationship with concepts of mortality and transcendence. This spiritual dimension shouldn’t be overlooked in treatment planning.
Creative expression becomes a vehicle for meaning-making. INFPs might write about their experience, create art inspired by their journey, or find new ways to express their evolving understanding of life and death. These creative outputs often become more meaningful to them than traditional markers of recovery.
Some INFPs discover a calling to help others facing similar challenges. Their natural empathy and deep processing of their own experience can translate into peer support, advocacy, or creative works that help other cancer patients. This sense of purpose can become a powerful healing force.
What Recovery Challenges Are Unique to INFPs?
Recovery for INFPs involves more than physical healing. They must integrate their cancer experience into their ongoing life narrative in a way that feels authentic and meaningful. This psychological integration can take longer than physical recovery and shouldn’t be rushed.
The transition from patient to survivor can be particularly challenging. INFPs might struggle with the expectation to “return to normal” when their experience has fundamentally changed their perspective on life. They need permission to emerge from treatment as a different person than they were before diagnosis.
Survivor’s guilt affects INFPs deeply when they know others with similar diagnoses who didn’t recover. Their empathetic nature makes it difficult to celebrate their own healing while others suffer. This can complicate their ability to fully embrace recovery and move forward.
Long-term follow-up care can trigger anxiety in INFPs who have developed hypervigilance about their health. Their Si function might become overactive, causing them to interpret normal body sensations as signs of recurrence. Learning to manage this health anxiety becomes crucial for quality of life.
Career and relationship changes following treatment can be complex for INFPs. They might feel called to make significant life changes based on insights gained during their cancer journey. However, these changes need to be implemented thoughtfully to avoid impulsive decisions that don’t serve their long-term well-being.
How Can Healthcare Providers Better Support INFP Patients?
Healthcare providers can significantly improve INFP patient experiences by understanding their unique psychological needs and communication preferences. Small adjustments in approach can make substantial differences in treatment compliance and emotional well-being.

Communication should prioritize authenticity over efficiency. INFPs respond better to providers who take time to understand their individual concerns and values rather than delivering standardized information. Personal connection, even in brief interactions, significantly impacts their trust and cooperation.
Treatment planning should include explicit discussion of how different options align with the patient’s values and life goals. INFPs need to understand not just what treatments are recommended, but why these recommendations make sense for their specific situation and priorities.
Scheduling flexibility helps accommodate INFP processing needs. When possible, major treatment decisions shouldn’t be required immediately. Providing written information they can review privately and offering follow-up appointments for questions supports their decision-making process.
Integrative care options should be presented when available. INFPs often benefit from complementary therapies that address their emotional and spiritual needs alongside medical treatment. This might include art therapy, meditation programs, or spiritual care services.
During my years managing complex client relationships, I learned that different personality types need different approaches to feel heard and supported. The same principle applies in healthcare. Understanding INFP preferences isn’t about special treatment, it’s about effective treatment that addresses their whole person, not just their medical condition.
Explore more INFP insights and personality-based approaches to life challenges in our complete MBTI Introverted Diplomats Hub.
About the Author
Keith Lacy is an introvert who’s learned to embrace his true self later in life. After running advertising agencies for 20+ years, working with Fortune 500 brands, and leading teams as an INTJ, Keith now helps introverts understand their personality and build careers that energize rather than drain them. His journey from trying to match extroverted leadership styles to embracing quiet leadership has taught him that authenticity isn’t just more fulfilling—it’s more effective. Through Ordinary Introvert, Keith shares insights on personality psychology, career development, and the power of understanding your true nature in a world that often misunderstands introversion.
Frequently Asked Questions
How do INFPs typically react to a prostate cancer diagnosis?
INFPs usually turn inward immediately after diagnosis, needing time to process the emotional and existential implications before engaging with treatment planning. Their dominant Introverted Feeling function creates an intense internal response that requires solitude and reflection to understand fully.
What makes treatment decisions particularly challenging for INFPs with cancer?
INFPs need treatment decisions to align with their core values and sense of authenticity, which doesn’t fit well with rushed medical timelines. They can’t simply analyze pros and cons logically but must feel that their choices are personally meaningful and consistent with their identity.
Why might traditional cancer support groups not work well for INFPs?
Large, structured support groups can feel artificial and draining to INFPs who prefer authentic, one-on-one connections. They benefit more from deep conversations with a few close supporters who can sit with their emotions without trying to fix or minimize them.
How do INFPs find meaning in their cancer experience?
INFPs integrate cancer into their life story and identity, often using the experience to clarify values and align their life more authentically. They might explore spirituality, engage in creative expression, or discover a calling to help others facing similar challenges.
What recovery challenges are unique to INFPs after cancer treatment?
INFPs struggle with expectations to “return to normal” when their experience has fundamentally changed their perspective. They need time for psychological integration and permission to emerge from treatment as a different person, which can take longer than physical recovery.